Your cardiologist’s report mentions PAD. The vascular surgeon’s notes say PVD. Your insurance paperwork uses both. You Google them and find articles treating them like they’re the same thing, except when they’re not.
This isn’t just medical jargon confusion. The distinction affects which specialist you see, what tests you need, and how your condition gets treated. Most people spend weeks trying to figure out if they even have the right diagnosis.
What Peripheral Vascular Disease Actually Means
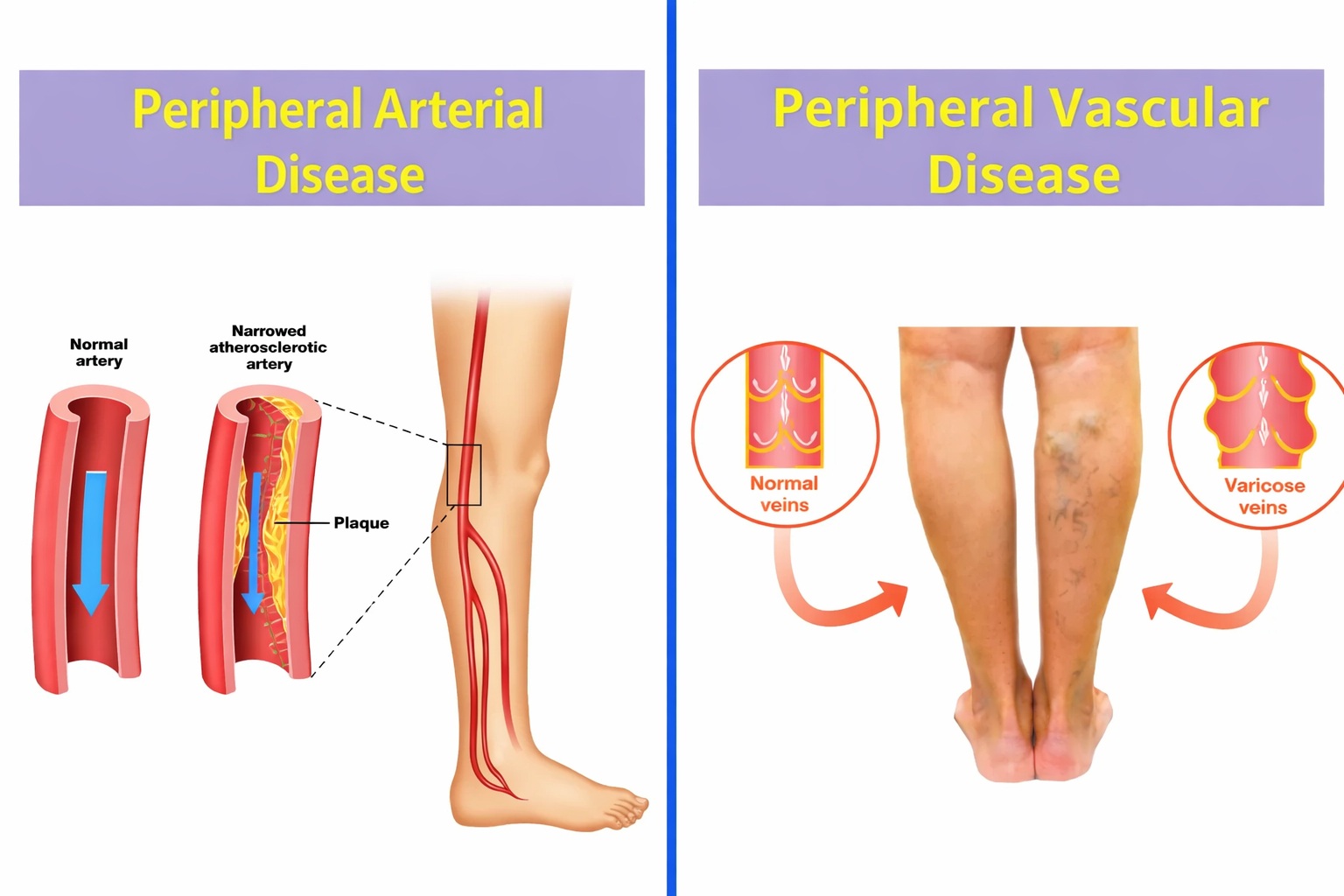
PVD is the catch-all term. It covers any blood vessel problem outside your heart and brain. Arteries, veins, lymphatic vessels, everything in your limbs.
Got varicose veins bulging in your legs? That’s PVD. Arteries narrowed by plaque? Also PVD. Blood clot in your calf? PVD again. The term itself tells you location (peripheral, meaning limbs) but nothing about which vessels or what’s wrong with them.
Think of PVD like saying “car trouble.” It confirms something’s broken but doesn’t specify whether it’s the engine, transmission, or brakes.
What Peripheral Arterial Disease Specifically Targets
PAD narrows the focus to arteries. The vessels pumping oxygen-rich blood from your heart to your legs, arms, and organs. Nothing to do with veins bringing blood back.
Plaque builds inside artery walls over decades. Cholesterol accumulates. Calcium hardens. The passageway shrinks. Blood flow drops. Your leg muscles start suffocating during activity because they’re not getting enough oxygen.
Walking two blocks makes your calves cramp. You stop. Pain vanishes within minutes. Start walking again. Same cramps at the same distance. That’s your arteries telling you they can’t deliver enough blood.
About 8-12 million Americans have PAD. Half don’t know it because they chalk up tired legs to getting older.
The Breakdown: PVD vs PAD
| PVD | PAD | |
| Scope | Any blood vessel problem in your limbs | Only artery problems |
| Vessels involved | Arteries, veins, lymphatic | Arteries exclusively |
| What causes it | Depends (could be clots, valve failure, plaque) | Atherosclerosis (plaque buildup) |
| Typical symptom | Varies wildly by vessel type | Leg cramping when walking that stops with rest |
| Examples | Varicose veins, DVT, artery narrowing | Clogged leg arteries, arm artery blockage |
Every case of PAD is PVD. But most PVD isn’t PAD.
What PAD Feels Like
Symptoms sneak up slowly. Most people ignore them for months, thinking they’re just out of shape.
Your calves cramp after walking three blocks. Rest fixes it temporarily. Pain returns at the same distance every time. That’s claudication, the textbook PAD symptom that many people confuse with general leg pain from other causes.
One foot feels colder than the other. Cuts on your toes heal slowly or not at all. Toenails grow slower. Leg hair thins out. Your leg looks shiny and smooth where hair stopped growing.
Common signs:
- Cramping in calf, thigh, or buttock during walking
- Coldness in one lower leg or foot
- Numbness or weakness in legs
- Sores on toes or feet that won’t close
- Color changes (pale or bluish) in legs
- Weak pulse in feet
Why Arteries Get Blocked
Atherosclerosis starts decades before symptoms appear. Cholesterol particles stick to artery walls. Immune cells try cleaning up the mess but get stuck themselves. Calcium deposits harden everything into plaque.
The biggest triggers:
- Smoking (accelerates plaque buildup by years)
- Diabetes (damages artery walls, making plaque stick easier)
- High blood pressure (creates tears in arteries where plaque lodges)
- High cholesterol (provides raw material for plaque)
- Age over 50 (more time for damage to accumulate)
- Family history (genetic factors affect how arteries handle cholesterol)
People with diabetes develop PAD 5-10 years earlier than those without. Smokers get it a full decade sooner than non-smokers, according to American Heart Association data.
Getting Diagnosed
The ankle-brachial index takes 10 minutes. Blood pressure cuff on your arm. Another on your ankle. Compare the numbers. If ankle pressure is significantly lower, blood isn’t reaching your feet properly.
ABI under 0.9 suggests PAD. Under 0.5 means severe blockage.
Vascular ultrasound shows exactly where arteries narrow and how badly. Sound waves create real-time images of blood flow. No needles, no radiation, no pain.
CT or MR angiography maps every artery in your legs when surgery is being considered. These scans guide precise treatment planning.
Treatment Approaches That Work
Lifestyle changes sound boring but they work better than most people expect. Walking programs build new tiny blood vessels around blockages. Your body literally creates detour routes for blood flow.
Thirty minutes of walking daily, even if you need to stop and rest multiple times, improves symptoms within 3-6 months. Regular walking strengthens leg circulation by forcing your body to develop new pathways around narrowed arteries. This isn’t optional. It’s the foundation of PAD treatment.
Quitting smoking matters more than any medication. Continuing to smoke while treating PAD is like bailing water from a boat with holes you refuse to patch.
Medications that help:
- Cilostazol improves walking distance by relaxing artery walls
- Antiplatelet drugs (aspirin or clopidogrel) prevent clots
- Statins slow plaque growth and stabilize existing buildup
- Blood pressure meds improve overall circulation
Procedures for severe cases:
- Angioplasty balloons open crushed arteries
- Stents hold problem areas open
- Atherectomy scrapes plaque from artery walls
- Bypass surgery routes blood around blocked sections
Most people avoid procedures by catching PAD early and sticking with lifestyle changes.
Stopping PAD Before It Starts
Prevention beats treatment. Always.
Never smoke. If you smoke, quit. That’s the single biggest thing you can do for your arteries. Exercise doesn’t have to mean gym memberships. Walking counts. Gardening counts. Taking stairs counts.
Blood sugar control matters enormously if you’re diabetic. Every point your A1C stays above 7% increases PAD risk. The same goes for blood pressure over 130/80 and LDL cholesterol over 100.
Recognizing early circulation warning signs helps catch problems before they become serious.
See a vascular specialist when:
- Leg pain appears with walking and disappears with rest
- Sores on feet or toes won’t heal after 2-3 weeks
- One leg feels noticeably colder than the other
- Foot pulses feel weak or absent
- You’re over 50 with diabetes, smoking history, or high blood pressure
Waiting to see if symptoms improve on their own wastes time. PAD caught at the cramping stage responds to walking and medication. PAD caught at the non-healing wound stage often needs procedures.
Common Questions
Is PAD the same as poor circulation?
PAD is one cause of poor circulation, specifically in arteries. Poor circulation can also come from vein problems, blood clots, or other conditions. PAD specifically means arterial narrowing from plaque.
What’s the main difference between PAD and varicose veins?
PAD affects arteries carrying oxygen to your legs. Varicose veins affect veins bringing blood back to your heart. Different vessels, different problems, different treatments.
Why do my legs cramp at night if I have PAD?
Advanced PAD causes rest pain because your tissues aren’t getting enough oxygen even when you’re lying down. This differs from common nighttime leg cramps that usually come from muscle fatigue or dehydration.
Getting Clear on Your Diagnosis
Knowing whether your leg problems stem from arteries, veins, or both changes everything about your treatment. PAD requires plaque management and blood flow improvement. Vein disease needs completely different approaches.
The confusion about PVD versus PAD keeps too many people from getting proper care. If your legs hurt when you walk, wounds won’t heal, or circulation feels off, that deserves evaluation now.
At Prime Vascular Care, we diagnose and treat all forms of peripheral vascular disease, with particular expertise in peripheral arterial disease. Schedule an evaluation to find out exactly what’s affecting your circulation and what will actually help.